Replies to post #150633 on Tornado Alley (PROG)

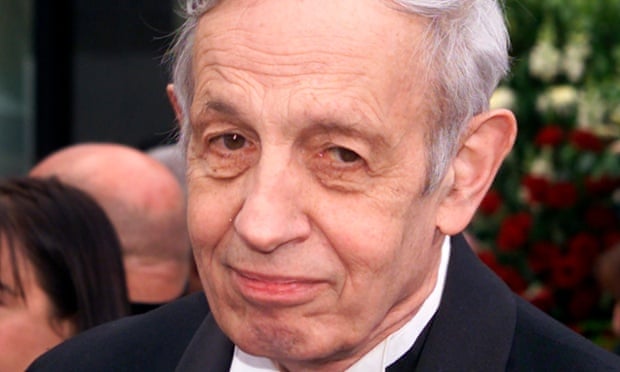
.. his condolences on Sunday morning.Stunned...my heart goes out to John & Alicia & family.
— Russell Crowe (@russellcrowe) May 24, 2015
An amazing partnership. Beautiful minds, beautiful hearts. https://t.co/XF4V9MBwU4
.. on its official Twitter account.NSA is saddened by the loss of famed mathematician John Nash. #nashletters http://t.co/5WmhcLVdSq
— NSA/CSS (@NSAGov) May 24, 2015




| Volume | |
| Day Range: | |
| Bid Price | |
| Ask Price | |
| Last Trade Time: |